What is Perthes Disease?

What is Perthes Disease?
Perthes Disease (also known as Legg-Calvé-Perthes Disease or LCPD) is a childhood condition that affects the hip joint, causing loss of blood flow to the femoral head (the ball part of the hip joint). Without sufficient blood supply, thefemoral head can become weak, leading to bone necrosis (bone death) and eventual collapse of the femoral head. Over time, the bone may gradually revascularise (regain blood flow), but this process can lead to deformity and joint damage, particularly if not treated appropriately.
Perthes Disease typically affects children between the ages of 4 and 10 years and is more common in boys than girls. The condition can affect one or both hips, but it is most commonly seen in just one hip.

Perthes Disease typically affects children between the ages of 4 and 10 years and is more common in boys than girls. The condition can affect one or hips, but it is most commonly seen in just one hip.
Causes of Perthes Disease
The exact cause of Perthes Disease is not known, but several factors may contribute to the condition:
Disruption of blood supply: The most significant factor in Perthes is reduced blood flow to the femoral head, causing it to weaken and collapse.

Genetics: There may be a genetic predisposition to Perthes, although it is not inherited in a simple manner.

Environmental factors: Trauma or previous injury to the hip may increase the risk of developing the condition.

Blood clotting disorders: In some cases, Perthes has been linked to disorders that affect blood clotting or circulation.
Symptoms of Perthes Disease
The symptoms of Perthes Disease can vary from mild to severe and may develop gradually. Common symptoms include:
Hip or groin pain, which may worsen with activity and improve with rest.
Limping or an altered gait (walking pattern).
Stiffness or reduced range of motion in the hip joint.

Thigh or knee pain, as the pain, may sometimes radiate down the leg.
Pain that worsens with physical activity, such as walking, running, or playing.
In the early stages, Perthes may not be immediately diagnosed, as the symptoms can be mistaken for other common childhood injuries, such as a muscle strain or hip sprain.

Diagnosis of Perthes Disease
To diagnose Perthes Disease, the following steps are typically involved:
Physical Examination: A healthcare professional will assess the child’s hip for signs of pain, tenderness, limited range of motion, and changes in gait.

X-rays: Imaging is essential to visualise the degree of femoral head collapse and joint damage. X-rays are typically the first step in confirming the diagnosis.

MRI or CT Scans: In some cases, MRI or CT scans may be used to better assess the extent of the damage and identify the stage of the disease.

Stages of Perthes Disease
Perthes Disease progresses in stages, which can range from the initial loss of blood flow to the eventual healing and reshaping of the femoral head. These stages include:
Initial stage (Inflammatory phase): Decreased blood flow to the femoral head, causing pain and inflammation.
Fragmentation stage: The femoral head weakens and starts to break apart, leading to collapse.
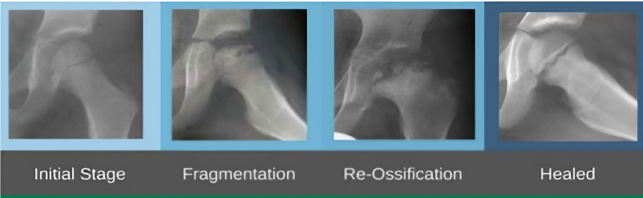
Re-ossification stage: The bone begins to heal, with new bone growth. This stage can take months or years.
Healing stage: The femoral head reforms, although it may not return to its original shape, which can lead to long-term hip problems.
Treatment of Perthes Disease
The goal of treatment for Perthes Disease is to manage pain, preserve the hip joint, and prevent long-term damage. Treatment varies based on the child’s age, the severity of the condition, and the stage of the disease.
Non-Surgical Treatment (Conservative Treatment)
For many children, particularly those in the early stages or with mild symptoms, non-surgical management can be effective in managing Perthes Disease:
Rest and Activity Modification: Encouraging rest and reducing activities that put stress on the hip joint (e.g., running, jumping) can help manage pain and prevent further joint damage.

Pain Management: Anti-inflammatory medications (e.g., ibuprofen) or acetaminophen can be used to manage pain and swelling associated with the condition.

Physical Therapy: Physiotherapy may be recommended to strengthen the muscles around the hip, improve mobility, and enhance the child’s ability to move without pain. A physiotherapist may also help with exercises to increase the range of motion.

Bracing or Splints: In some cases, a brace or splint may be used to keep the hip in a stable position while it heals, particularly in younger children.

Surgical Treatment
In more severe cases of Perthes Disease, or if the femoral head becomes misshapen and unstable, surgery may be needed to prevent long-term complications such as arthritis or deformity. Surgical options include:
Femoral Osteotomy: This procedure involves cutting and realigning the femur to improve the alignment of the femoral head within the acetabulum (hip socket). This may help distribute pressure more evenly across the joint and allow for better healing.

Pelvic Osteotomy: In some cases, the acetabulum (hip socket) may need to be repositioned to improve coverage of the femoral head. This surgery is more complex and is usually reserved for older children or those with significant hip deformities.

Total Hip Replacement: In rare cases where the hip joint has suffered severe damage and arthritis is present, particularly in adolescents, hip replacement surgery may be considered.

Why Choose Mr. Tahir Khan for Treatment of Perthes Disease?
Mr. Tahir Khan is a Consultant Orthopaedic Surgeon at the Royal National Orthopaedic Hospital (RNOH), specialising in paediatric and adolescent orthopaedic conditions, including Perthes Disease. He has extensive experience in managing Perthes Disease, from conservative management in younger children to advanced surgical techniques in older children and adolescents.
Mr. Khan’s approach to Perthes Disease is comprehensive and tailored to each individual patient, taking into account:
Age and severity of the disease: Mr. Khan uses a patient-centred approach to determine whether surgical or non-surgical treatment is best suited to your child’s needs.
Minimally invasive techniques: Where possible, he employs minimally invasive procedures to reduce recovery times, limit scarring, and ensure quicker rehabilitation.
Focus on long-term outcomes: His treatment approach prioritises long-term joint health and aims to preserve the hip joint and minimise the risk of arthritis or future surgery.
With access to the world-class facilities at RNOH and a dedicated team of paediatric specialists, Mr. Khan ensures that every child receives the highest standard of care for Perthes Disease
What to Expect During Treatment with Mr. Khan
Initial Consultation: Mr. Khan will perform a thorough examination of your child, review their medical history, and discuss the symptoms in detail. Imaging studies (X-rays, MRI, etc.) will be reviewed to determine the extent of the disease.

Treatment Plan: Based on the diagnosis and your child’s age, Mr. Khan will develop a tailored treatment plan. If non-surgical treatment is appropriate, this will involve rest, physiotherapy, and pain management. If surgery is needed, the procedure will be explained in detail, and preoperative tests will be conducted.

Surgical Intervention (if required): If surgery is necessary, Mr. Khan will perform the appropriate procedure using the latest techniques. Post-surgery, the child will be monitored closely for any signs of complications and will begin a rehabilitation program.
Follow-Up and Rehabilitation: Regular follow-up appointments will be scheduled to monitor progress and ensure the hip is healing well. Physiotherapy will play a key role in helping your child regain full mobility and strength in the hip joint.

Long-Term Care: Once healing is complete, Mr. Khan will continue to monitor your child’s hip development to ensure that they do not experience long-term complications like arthritis.
Contact Information
For more information or to schedule a consultation with Mr. Tahir Khan, please contact:
- Royal National Orthopaedic
- Portland
- Princess Grace
- Spire Bushey Hospital
